Gut Feelings Got Better: How I Fixed My Stomach Naturally and Actually Saw Results
Living with constant bloating, discomfort, and unpredictable digestion used to be my normal—until I realized I wasn’t alone. Millions struggle with stomach issues daily, often ignoring the root causes. What if small, science-backed changes could transform your gut health? This is not about quick fixes, but real, lasting optimization. Let me walk you through what actually worked. It wasn’t a miracle cure or a trendy diet, but a series of thoughtful, consistent choices grounded in how the body truly functions. The journey to better digestion begins not with restriction, but with understanding.
The Hidden Struggle: Why Stomach Discomfort Is More Common Than You Think
Digestive discomfort has become so common that many people accept it as an inevitable part of modern life. Bloating after meals, occasional acid reflux, irregular bowel movements—these are often brushed off as minor inconveniences. Yet, when experienced regularly, they signal deeper imbalances. According to global health surveys, up to 40% of adults report frequent gastrointestinal symptoms, with women over 30 being particularly affected. This widespread issue is not simply a result of aging, but a reflection of lifestyle patterns that have quietly eroded digestive resilience over time.
Modern eating habits play a major role. Processed foods high in refined sugars, unhealthy fats, and artificial ingredients dominate many households. These substances can disrupt the delicate balance of the gut microbiome—the trillions of beneficial bacteria that support digestion, immunity, and even mood regulation. At the same time, increased stress levels, sedentary routines, and irregular sleep further strain the digestive system. The body is designed to process whole, nutrient-dense foods in a calm environment, but today’s pace rarely allows for that.
Perhaps the most overlooked factor is the normalization of digestive distress. Many women in their 30s, 40s, and 50s come to expect bloating after meals or fatigue after eating as “just how it is.” This mindset delays meaningful change. When discomfort is dismissed, the opportunity to address root causes—such as poor food combinations, chronic stress, or hydration deficits—is lost. The first step toward improvement is recognizing that persistent stomach issues are not normal, nor should they be accepted as a lifelong burden.
What Your Gut Is Trying to Tell You: Understanding the Digestive System’s Signals
The digestive system is more than a food-processing tube—it is a complex network of organs, nerves, and microbes that communicate constantly with the brain. When you feel bloating, gas, or a burning sensation, these are not random events. They are signals, much like a warning light on a car’s dashboard. The stomach produces hydrochloric acid to break down food and protect against harmful bacteria. Enzymes from the pancreas and small intestine further digest proteins, fats, and carbohydrates. The gut lining acts as a barrier, allowing nutrients to pass into the bloodstream while keeping toxins and undigested particles out.
When any part of this system is compromised, symptoms arise. For example, low stomach acid—often mistaken for excess acid—can lead to poor digestion, bacterial overgrowth, and reflux. This misunderstanding leads many to rely on antacids, which may offer short-term relief but can worsen the problem over time by further reducing acid production. Similarly, a damaged gut lining, sometimes referred to as “leaky gut” in popular health discussions, may allow substances to enter the bloodstream that trigger inflammation. While this term is not a formal medical diagnosis, the underlying concept of intestinal permeability is supported by scientific research.
Another key player is the gut microbiome. A diverse and balanced microbial community supports efficient digestion, produces essential vitamins like B12 and K, and helps regulate the immune system. Disruptions from antibiotics, poor diet, or chronic stress can reduce this diversity, leading to gas, bloating, and irregularity. The gut also produces neurotransmitters such as serotonin, which explains why digestive issues often coincide with low mood or anxiety. Recognizing these connections helps shift the perspective from treating isolated symptoms to supporting the entire digestive ecosystem.
My Turning Point: When I Stopped Ignoring My Body’s Warnings
For years, I managed my digestive discomfort with over-the-counter remedies and avoidance. I would skip social dinners to prevent bloating, wear loose clothing, and excuse my low energy as a consequence of a busy schedule. But the turning point came during a family gathering when I couldn’t enjoy a meal with loved ones. I felt distended, sluggish, and disconnected. That moment of exclusion—missing out on a simple joy because of my stomach—was a wake-up call. I realized I was not just managing symptoms; I was letting them dictate my life.
The emotional toll was deeper than I had admitted. There was frustration at not understanding my own body, embarrassment when discomfort surfaced in public, and a quiet sense of defeat. I had tried various diets—low carb, intermittent fasting, detox teas—but none brought lasting relief. Each attempt left me more confused, often worse off. I began to question whether real improvement was possible without medication or extreme restriction. That’s when I shifted my focus from quick fixes to sustainable, science-aligned changes.
I decided to approach my gut health like a long-term project, not a crisis to be solved overnight. I consulted a registered dietitian who helped me understand my patterns without judgment. Instead of labeling foods as “good” or “bad,” we looked at timing, combinations, and lifestyle factors. This compassionate, evidence-based approach made all the difference. I stopped blaming myself and started observing. I tracked meals, energy levels, and symptoms. Within weeks, patterns emerged. I noticed that late-night eating, rushed meals, and high-sugar snacks consistently preceded discomfort. This awareness became the foundation for real change.
The Three Core Shifts That Changed Everything
With guidance and self-reflection, I identified three foundational changes that transformed my digestion. These were not drastic overhauls, but consistent, manageable adjustments. The first was **dietary timing**. I began eating within a 10- to 12-hour window each day, finishing dinner at least three hours before bedtime. This allowed my digestive system to rest and reset overnight. Research shows that giving the gut a break between meals supports motility and reduces fermentation, which can cause bloating. I also avoided eating while stressed or distracted, choosing instead to sit down, breathe, and focus on my food.
The second shift was **food quality**. I gradually reduced processed foods, especially those high in added sugars and refined carbohydrates. Instead, I prioritized whole, fiber-rich foods like vegetables, fruits, legumes, and whole grains. Fiber feeds beneficial gut bacteria and promotes regular bowel movements. I also increased my water intake, aiming for at least eight glasses daily. Hydration is essential for softening stool and supporting enzyme function. I didn’t eliminate any food group entirely—balance was key. Even occasional treats were fine, as long as they didn’t become the norm.
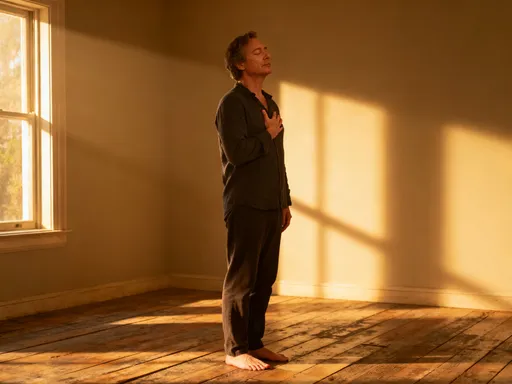
The third and perhaps most surprising change was **stress management**. I had always thought of stress as a mental issue, not a digestive one. But the gut-brain axis is real: stress signals from the brain can slow digestion, increase inflammation, and alter gut motility. I started incorporating simple practices like diaphragmatic breathing for five minutes each morning and taking a 20-minute walk after dinner. These small habits calmed my nervous system and, over time, improved my digestion. I also reduced screen time before bed, which enhanced sleep quality—a critical factor in gut repair.
Eating Smart: Practical Swaps That Support Stomach Health
Changing my diet didn’t require complicated recipes or expensive supplements. It was about making smarter, sustainable choices. One of the easiest swaps was replacing sugary snacks with whole fruits. Instead of reaching for cookies or candy in the afternoon, I chose an apple with a handful of almonds or a banana with a spoon of natural peanut butter. These combinations provide fiber, healthy fats, and natural sugars that stabilize blood sugar and reduce cravings. I also switched from white bread and pasta to whole grain versions, which contain more fiber and nutrients.
Another helpful change was incorporating fermented foods. I added plain yogurt with live cultures, kefir, sauerkraut, and kimchi in small amounts. These foods contain natural probiotics—beneficial bacteria that support gut balance. I didn’t overconsume them; a quarter-cup of sauerkraut or a small glass of kefir a few times a week was enough. I also learned to read labels, avoiding products with added sugars or preservatives that could negate the benefits. Probiotic supplements were an option, but I found food sources to be gentler and more effective for my system.
Portion control and eating pace made a significant difference. I used smaller plates and bowls to naturally reduce portion sizes. More importantly, I began chewing each bite thoroughly—aiming for 20 to 30 chews per mouthful. This simple act improved digestion by breaking down food mechanically and signaling the stomach to prepare for incoming nutrients. Eating slowly also allowed my brain time to register fullness, preventing overeating. I made meals a quiet time, turning off the TV and putting away my phone. This mindful approach reduced digestive strain and increased satisfaction.
Beyond Food: Sleep, Movement, and Their Gut Connection
Digestive health extends far beyond the plate. Sleep, in particular, plays a crucial role. During deep sleep, the body repairs tissues, balances hormones, and restores the gut lining. Chronic sleep deprivation disrupts the circadian rhythm, which regulates digestive enzyme release and gut motility. I noticed that on nights when I slept poorly, my digestion the next day was sluggish. To improve sleep, I established a consistent bedtime and created a wind-down routine: dimming lights, drinking herbal tea, and reading a book. I also kept my bedroom cool and free of electronic distractions.
Movement was another key factor. While intense exercise can sometimes aggravate digestion, gentle physical activity supports it. I started taking a 15- to 20-minute walk after meals, which helped stimulate gastric emptying and reduce bloating. Daily movement also reduced stress and improved circulation, both of which benefit gut function. I didn’t need a gym membership—simple activities like gardening, stretching, or dancing in the kitchen were enough. The goal was consistency, not intensity. Over time, my energy improved, making it easier to stay active without feeling drained.
Hydration remained a constant focus. I carried a reusable water bottle and set reminders to drink throughout the day. I also included water-rich foods like cucumbers, watermelon, and oranges. Proper hydration supports mucosal lining in the gut and prevents constipation. I avoided drinking large amounts during meals, as this can dilute stomach acid. Instead, I sipped water between meals and had a glass first thing in the morning to kickstart digestion. These small habits, when combined, created a supportive environment for optimal gut function.
Sustainable Results: How Small Consistency Beats Extreme Diets
The improvements didn’t happen overnight. It took about eight to ten weeks before I noticed consistent changes. Bloating became less frequent, energy levels stabilized, and I no longer dreaded meals. I didn’t achieve perfection—occasional discomfort still occurred, especially during stressful periods or travel—but my baseline had shifted. I felt more in tune with my body, able to recognize early signs of imbalance and respond with simple adjustments.
One of the most valuable lessons was rejecting the all-or-nothing mindset. I used to think that unless I followed a strict plan perfectly, I had failed. But sustainable health is not about perfection. It’s about progress, flexibility, and self-compassion. I allowed myself occasional indulgences without guilt, knowing that one meal wouldn’t undo weeks of consistent care. I also learned to listen to my body’s signals—when to eat, when to rest, when to move. This intuitive approach felt more natural and empowering than any rigid diet ever had.
Sharing my experience with friends, I realized many had similar struggles. Some had tried extreme cleanses or eliminated entire food groups, only to regain symptoms later. My approach wasn’t flashy or marketed as a cure-all, but it worked because it was rooted in balance and science. I didn’t lose weight rapidly or make dramatic claims. Instead, I gained something more valuable: daily comfort, mental clarity, and the freedom to enjoy life without digestive fear.
Rethinking Stomach Health as a Daily Practice
Looking back, the journey to better gut health was not about fixing a broken system, but nurturing one that had been neglected. It required patience, observation, and a willingness to change small habits over time. The digestive system is resilient, but it needs consistent support—quality food, adequate rest, movement, and emotional calm. When these elements align, the body responds with greater energy, improved mood, and fewer disruptions.
Gut health is not a destination, but a daily practice. It’s choosing a piece of fruit over a processed snack, taking a moment to breathe before eating, or going to bed at a reasonable hour. These choices may seem small, but their cumulative effect is profound. They reflect a deeper commitment to self-care—one that honors the body’s wisdom and capacity for healing.
If you’re living with ongoing digestive discomfort, know that you’re not alone, and you don’t have to accept it as normal. Start with one change—perhaps drinking more water, eating slower, or taking a short walk after dinner. Track how you feel. Be patient. Progress is rarely linear, but every step counts. And while this journey is personal, it doesn’t have to be taken alone. Consulting a healthcare provider or registered dietitian can offer guidance tailored to your needs. True wellness begins not with drastic measures, but with gentle, consistent care—because a healthier gut means a more vibrant, joyful life.