How I Found Myself Again After Baby — Simple Changes That Actually Worked
After giving birth, I felt like a stranger in my own body and routine. The exhaustion, emotional ups and downs, and lost sense of identity were real. But instead of chasing quick fixes, I focused on small, sustainable lifestyle shifts that honored my recovery. This isn’t about bouncing back — it’s about moving forward with more balance, energy, and self-trust. These changes didn’t just help me heal; they reshaped how I live every day. Healing after childbirth is not a linear process, nor is it one-size-fits-all. It’s layered, deeply personal, and often underestimated in a culture that glorifies speed and productivity. For many women, the postpartum period becomes a silent struggle masked by smiles and swaddled babies. Yet beneath the surface, bodies are rebuilding, hormones are recalibrating, and identities are quietly reshaping. This journey is not about returning to who you were — it’s about discovering who you are becoming, with compassion, intention, and time.
The Hidden Challenge of Postpartum Life
Childbirth is one of the most transformative experiences a woman can go through, yet the weeks and months that follow are often treated as an afterthought. While much attention is given to labor and delivery, the true test of resilience comes afterward — in the quiet, sleepless hours when the world expects you to adapt instantly. The physical recovery alone can be immense: stretched tissues, hormonal fluctuations, and the gradual return of strength and stamina. But beyond the body, there’s a psychological shift that rarely gets discussed — the loss of self. Many women report feeling disconnected from their pre-baby identity, unsure of where they fit in their new reality. They are mothers now, yes, but who are they beyond that role?
Society often sends the message that recovery should be swift and invisible. Social media feeds are filled with images of women “snapping back” within weeks, reinforcing the idea that strength means bouncing back quickly. But this narrative overlooks the biological truth: healing takes time. The uterus needs six to eight weeks to return to its pre-pregnancy size. Hormones like estrogen and progesterone plummet after delivery, which can affect mood, sleep, and energy levels. The pelvic floor, which has supported the weight of a growing baby for months, requires careful rehabilitation. Yet, these processes are rarely acknowledged in everyday conversations about motherhood. Instead, women are praised for doing it all — caring for a newborn, managing a household, and looking put-together — without recognizing the toll it takes.
What’s more, the emotional landscape of postpartum life is complex. Feelings of joy may coexist with grief — grief for the freedom of the past, for the body that once felt familiar, for the simplicity of life before responsibility multiplied overnight. These emotions are normal, yet they are often minimized or dismissed as “just hormones.” True recovery must include space for these feelings, not just the physical repair of tissues. It requires a shift in mindset — from performance to presence, from comparison to self-compassion. Recognizing that healing is not just skin deep, but woven into the mental, emotional, and spiritual fabric of a woman’s life, is the first step toward a more honest and sustainable recovery.
Why Slow Healing Is Actually Smart Healing
In a world that values speed and efficiency, the idea of slowing down during recovery can feel counterintuitive. Many women feel pressure to return to their pre-pregnancy weight, resume workouts, and re-enter social life as quickly as possible. But maternal health experts consistently emphasize that rushing the postpartum period can lead to long-term consequences. The body has undergone a significant physiological event — childbirth — and it needs time to heal properly. Just as a broken bone requires weeks to mend, the internal changes from pregnancy and delivery need time to resolve. Tissues that have stretched, such as the abdominal wall and pelvic floor, need time to regain strength. Hormonal systems need time to rebalance. The nervous system, often in a heightened state from labor and newborn care, needs time to reset.
Research in maternal physiology shows that the first 12 weeks postpartum are critical for foundational healing. During this time, the body is still processing the massive hormonal shifts that occur after delivery. Prolactin, which supports milk production, remains elevated, while estrogen and progesterone drop sharply. This hormonal shift can affect mood, libido, and energy levels. Additionally, the connective tissue that held the expanding uterus — including the linea alba, the tissue between the abdominal muscles — is often weakened. Rushing into intense exercise or heavy lifting during this period can increase the risk of complications such as diastasis recti (abdominal separation) or pelvic organ prolapse.
Experts recommend a gradual, phased approach to recovery. In the first six weeks, the focus should be on rest, nourishment, and gentle movement. From six to twelve weeks, women can begin to reintroduce strength and stability exercises under professional guidance. After twelve weeks, a more comprehensive movement routine can be considered — but only if the body signals readiness. This phased model isn’t about limitation; it’s about respect. It honors the body’s natural timeline and prioritizes long-term health over short-term appearance. When women allow themselves to heal at their own pace, they build a stronger foundation for future energy, strength, and resilience. Slow healing isn’t laziness — it’s wisdom.
Rest That Goes Beyond Sleep
When most people think of rest, they imagine sleep — lying down, closing the eyes, and escaping into unconsciousness. But for new mothers, even sleep doesn’t always feel restorative. The reality is that true recovery requires more than just hours logged in bed. It requires active rest — intentional moments of stillness, breath, and nervous system regulation. Active rest is not passive. It’s a deliberate practice of giving the body and mind space to reset, repair, and recharge. This kind of rest supports cellular repair, reduces inflammation, and helps regulate mood and energy levels.
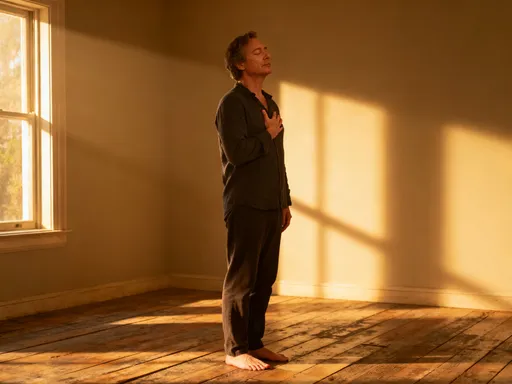
One of the most effective forms of active rest is diaphragmatic breathing — slow, deep breaths that engage the diaphragm and activate the parasympathetic nervous system, the body’s “rest and digest” mode. Just five minutes of focused breathing several times a day can lower cortisol levels, improve oxygen flow, and calm the mind. Another powerful tool is mindful stillness — sitting quietly, even for a few minutes, without distraction. This doesn’t require meditation expertise. It can be as simple as sitting with a cup of tea, feeling the warmth, noticing the breath, and letting thoughts come and go without judgment.
Finding time for these practices in a chaotic newborn schedule may seem impossible, but small moments add up. A mother can practice deep breathing while feeding her baby. She can pause for 60 seconds between tasks to close her eyes and reset. She can place her hand on her lower abdomen and gently reconnect with her core. These micro-moments of recovery are not luxuries — they are essential. They signal to the body that it is safe, supported, and not in constant survival mode. Over time, this nervous system regulation enhances physical healing, improves sleep quality, and increases emotional resilience. Rest, when done intentionally, becomes one of the most powerful tools in postpartum recovery.
Eating to Rebuild, Not Restrict
In the aftermath of childbirth, nutrition plays a vital role in recovery — yet many women are tempted to focus on weight loss rather than healing. This mindset can be counterproductive. The body needs energy and nutrients to repair tissues, produce breast milk, and stabilize mood. Restrictive diets, especially in the early postpartum months, can deprive the body of essential vitamins and minerals, leading to fatigue, weakened immunity, and slower recovery. Instead of restriction, the focus should be on rebuilding — on fueling the body with nutrient-dense foods that support long-term health.
Protein is one of the most important nutrients during recovery. It supports tissue repair, hormone production, and muscle rebuilding. Including a source of high-quality protein at every meal — such as eggs, Greek yogurt, lentils, or lean meat — can help stabilize blood sugar and sustain energy. Iron is another critical nutrient, especially for women who experienced blood loss during delivery. Low iron levels can contribute to fatigue and low mood, so incorporating iron-rich foods like spinach, lentils, and red meat, along with vitamin C to enhance absorption, is beneficial. Hydration is equally important. Breastfeeding increases fluid needs, and even mild dehydration can affect energy and cognitive function. Simple habits — like keeping a large water bottle nearby, adding lemon for flavor, or drinking herbal teas — can make hydration easier to maintain.
Meal planning doesn’t have to be complicated. Batch cooking on low-energy days, using frozen vegetables, and preparing simple one-pan meals can reduce stress and ensure consistent nourishment. The goal is not perfection, but consistency. Eating regular, balanced meals sends a message to the body that it is valued and supported. It’s also important to listen to hunger and fullness cues. Intuitive eating — honoring what the body needs rather than following rigid rules — fosters a healthier relationship with food and reduces the risk of disordered eating patterns. Nutrition during postpartum should be about nourishment, not punishment. When women eat to rebuild, they give their bodies the tools they need to heal from the inside out.
Movement That Feels Good, Not Punishing
Movement is a key component of postpartum recovery, but the type and timing matter greatly. Many women feel pressure to return to intense workouts quickly, often drawn by fitness trends or social media influencers. However, jumping into high-impact exercise too soon can do more harm than good. The body needs time to reestablish foundational strength, particularly in the core and pelvic floor. Without proper preparation, activities like running or heavy lifting can increase the risk of pelvic floor dysfunction, including urinary incontinence and organ prolapse.
Gentle, progressive movement is the safest and most effective approach. Walking is one of the best starting points — it’s low-impact, accessible, and supports circulation, mood, and digestion. Even short walks around the block, with the baby in a carrier, can make a difference. Stretching and mobility work help release tension in areas that may have tightened during pregnancy, such as the hips, lower back, and shoulders. Diaphragmatic breathing, when coordinated with movement, helps retrain the core muscles and improve intra-abdominal pressure management.
Core reactivation is especially important. During pregnancy, the abdominal muscles stretch and the linea alba widens. After delivery, these tissues need to be re-engaged gradually. Exercises like pelvic tilts, gentle abdominal drawing-in maneuvers, and supported bridges can help rebuild core strength without strain. It’s essential to avoid traditional crunches or sit-ups in the early months, as these can exacerbate diastasis recti. Working with a pelvic floor physical therapist can provide personalized guidance and ensure safe progression. The goal of postpartum movement is not to burn calories, but to reconnect with the body, restore function, and build confidence. When movement feels good — supportive, energizing, and sustainable — it becomes a form of self-care, not punishment.
Building a Realistic Daily Rhythm
One of the most powerful tools in postpartum recovery is consistency — not intensity. Establishing a realistic daily rhythm can bring stability to an otherwise chaotic time. This doesn’t mean rigid schedules or perfection. It means creating small, repeatable habits that support physical and emotional well-being. Morning light exposure, for example, helps regulate the circadian rhythm, which can improve sleep and mood. Simply stepping outside for five minutes with a cup of tea can signal to the body that a new day has begun.
Meal prep shortcuts can reduce decision fatigue. Pre-chopping vegetables, using canned beans, or preparing overnight oats can make healthy eating more manageable on low-energy days. Baby-wearing walks combine movement, fresh air, and bonding — all in one activity. Even small rituals, like washing the face each morning or changing into daytime clothes, can create a sense of normalcy and self-respect.
Partners and caregivers can play a crucial role in supporting these rhythms. Simple acts — holding the baby while the mother showers, preparing a snack, or taking over a feeding with expressed milk — can provide meaningful relief. The goal is not to do everything alone, but to build a supportive environment where recovery is prioritized. These small, consistent actions accumulate over time, creating a foundation of stability that makes long-term health more achievable. Recovery is not about dramatic changes — it’s about showing up, day after day, with kindness and intention.
Emotional Recovery: Making Space for All the Feels
Emotional healing is just as important as physical recovery, yet it often goes unaddressed. The postpartum period is marked by a wide range of emotions — joy, love, overwhelm, sadness, guilt, and sometimes grief. These feelings are not signs of weakness; they are signs of being human. Hormonal shifts, sleep deprivation, and the magnitude of life change all contribute to emotional volatility. But when women are encouraged to “just be happy” or “enjoy every moment,” they may feel pressured to suppress difficult emotions, which can lead to isolation and burnout.
Creating space for emotional expression is essential. Journaling can be a powerful tool — writing down thoughts and feelings without judgment helps process emotions and gain clarity. Talking circles, whether with friends, family, or support groups, provide connection and validation. Therapy, when accessible, offers a safe space to explore identity shifts, relationship dynamics, and mental health concerns. Even simple practices — like naming emotions out loud (“I’m feeling overwhelmed right now”) — can reduce their intensity and create a sense of control.
Emotional wellness is not a luxury; it is foundational to full recovery. When women feel seen and heard, they are more likely to seek help, set boundaries, and practice self-compassion. Normalizing the full spectrum of postpartum emotions — not just the joyful ones — helps dismantle the myth of the “perfect mother.” Healing includes tears as much as laughter, silence as much as conversation. By honoring all the feels, women can rebuild not just their bodies, but their sense of self.
Postpartum recovery isn’t a race or a checklist. It’s a quiet rebuilding of body, mind, and rhythm — one small choice at a time. By choosing simplicity over speed, and self-care over performance, women can emerge not just healed, but stronger, wiser, and more connected to themselves. The journey is not about returning to who you were, but about growing into who you are becoming. Each small act of rest, nourishment, movement, and emotional honesty is a step toward wholeness. Always consult a healthcare provider before starting any recovery plan — because real healing happens best with support.